A new federal initiative, the Rural Health Transformation Program, aimed at stabilizing health systems in underserved, rural regions, is budgeted for $50 billion. According to the Centers for Healthcare Quality and Payment Reform, Indiana has 52 rural hospitals as of 2024, and 25% of those have already cut back services.
The program, set to begin in fiscal year 2026, will allocate $10 billion annually for five years to states that develop approved rural health transformation plans. Half the money will be distributed evenly among participating states, while the remainder will be awarded based on rural population and need.
The rural health program was added to a broader budget package that includes sweeping reductions in Medicaid funding. The Congressional Budget Office estimates federal Medicaid spending will be reduced by approximately $1 trillion over the next decade. Rural areas alone are expected to lose $155 billion in funding.
“We are collaborating with Indiana Family and Social Services Administration (FSSA) to help frame how the Rural Health Transformation Fund could create the best impact for our rural health care organizations,” said Cara Veale, DHS, FACHE, the CEO of the Indiana Rural Health Association.
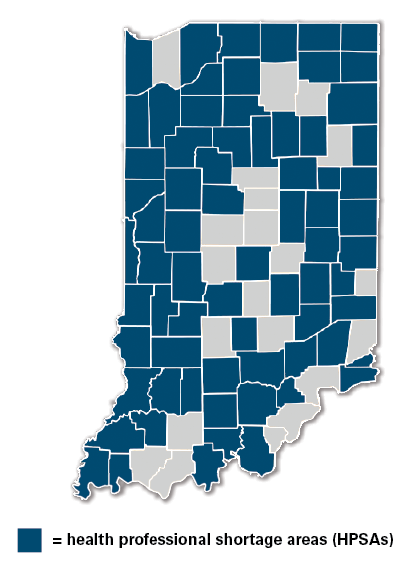
According to the Cicero Institute, one in five Indiana residents relies on Medicaid, and 71 of Indiana’s 92 counties face physician shortages. Indiana’s population is approximately 30% rural, and rural residents are more likely to have chronic conditions and live in poverty. The same study calculates that as many as 2,033,082 Indiana residents are living in underserved areas.
The rural health program requires states to submit a detailed rural transformation plan by the end of the year, outlining efforts to expand access, improve outcomes, upgrade technology, and retain health care workers. However, the implementation process remains unclear.
Indiana’s top concerns are in step with the social determinants of health. However, Veale points out, “Every rural community has their own challenges.”
Restoring emergency, birthing, and mental health services is at the top of the list for many hospitals. Also, enhancing Medicaid reimbursement rates is a concern. The state is currently among the lowest in the Midwest with average base payment around $3,524 per inpatient stay, compared to $5,000 or more in Kentucky and Ohio. Looking toward the future, investments in telehealth, cybersecurity, and recruitment initiatives will prove to be important, as will protections for rural health clinic funding and Medicaid coverage.
“If you are specifically looking at what challenges rural hospitals and health care organizations experience, funding is likely the biggest challenge,” Veale said. “Rural health care organizations typically see a larger portion of patients on government-supported insurance (Medicare and Medicaid), which tends to reimburse below the cost to provide the service.”
The law calls for Centers for Medicare & Medicaid Services (CMS) Administrator Mehmet Oz, MD, MBA, to distribute the population-based portion of the funds. The CMS has not specified how states should apply or what metrics will determine funding levels.