by Carol Hoppe, CPC, CCS-P, CPC-I
MedLucid Solutions, LLC
Since the mid-1990s, physicians have been coding for Evaluation and Management (E/M) services based on three key components:history, exam and medical decision making (MDM). Time could also be a factor when greater than 50% was spent in counseling and/or coordination of care.
These guidelines, especially with regard to MDM, have been vague and interpreted in various ways over the last 25 years. Some payers have relied on the Marshfield Clinic Tool; some Medicare carriers have provided their own tools. Here in Indiana, our Medicare carrier has given us no written guidelines for how they interpret the MDM key component other than the Table of Risk (which is only one of three elements in MDM). We know that medical necessity is the overarching criteria for determining the appropriate level of service, but what does that mean when it comes to documentation?
CMS decided to alter the E/M guidelines in 2018 as part of the Patients Over Paperwork Act. Since then, the AMA has been working to create a new set of E/M guidelines that will become effective Jan. 1, 2021.
Here are five things you should know about the new coding guidelines:
1.
Changes only apply to office or other outpatient codes 99202-99215. Code 99201 has been removed, as the MDM was the same as 99202. The new guidelines do not apply to any other E/M services, such as hospital, emergency room or nursing facility codes.
2.
History and exam elements are no longer required for code selection.
3.
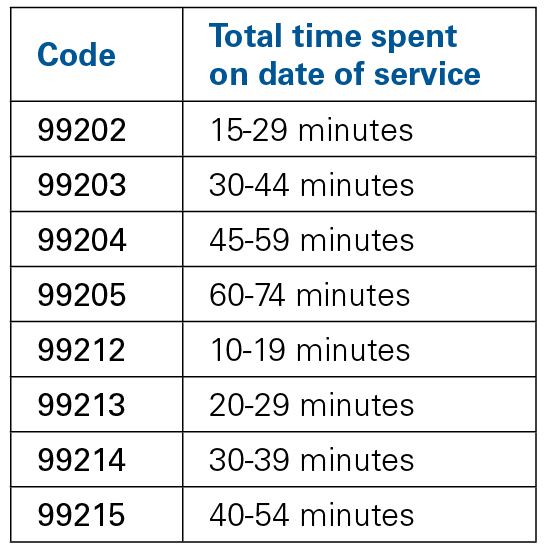
Coding can be based on MDM or time, with new times for each E/M code.
4.
Time now represents total provider time spent on the date of service, including:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
5.
MDM and the Table of Risk have been revised, including:
- Removed ambiguous terms (e.g. “mild”) and defined previously ambiguous concepts (e.g. “acute or chronic illness with systemic symptoms”).
- Also defined important terms, such as “independent historian.”
- Redefined the data element to move away from simply adding up tasks to focusing on tasks that affect the management of the patient (e.g. independent interpretation of a test performed by another provider and/or discussion of test interpretation with an external physician/QHP).
During COVID-19, telehealth services can now be based on some of the 2021 guidelines, but not all of them. The first four items are approved for coding during the public health emergency (PHE); however, the changes to MDM and the Table of Risk are not yet effective. When using MDM for code selection, physicians should continue to select the level of service based on the current 1995/1997 MDM guidelines during the PHE.
For more information on E/M changes for 2021, visit the AMA website
here and
here. Several ISMA webinars on billing and coding for telehealth during COVID-19 are available on the ISMA Online app; download it
here.
Learn more in upcoming ISMA webinars
ISMA is planning three CME webinars with Carol Hoppe on the billing and coding topics below.
If you have specific questions you’d like us to answer during these sessions, email Jessica Davis
at jdavis@ismanet.org.
2021 ICD-10-CM updates
Sept. 3, 11 a.m. to noon
2021 CPT updates
December, TBD
2021 E/M updates
December, TBD |